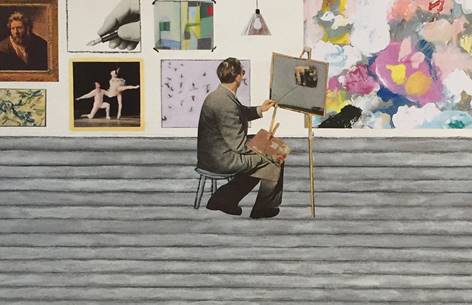
 For too long, old age has been associated with negative images, words, and ideas. This special report from NextAvenue—public media’s first and only outlet dedicated to older adults—examines the vitality, excitement, and joy that comes to those who connect aging and art. Learn more here.
For too long, old age has been associated with negative images, words, and ideas. This special report from NextAvenue—public media’s first and only outlet dedicated to older adults—examines the vitality, excitement, and joy that comes to those who connect aging and art. Learn more here.
This post and the original special report first appeared on NextAvenue.org.